The vital capacity (VC) is one of the main parameters used to assess lung functions and capacity, providing basic visions about the effectiveness of the lungs that you can keep and expel air. This measurement is crucial in diagnosing and monitoring various pulmonary cases.
Unlike forced maximum capacity, the expiration of the validity is performed as soon as possible, the expiration of the validity during the vital capacity is not accelerated. Instead, this is done as much as possible, ensuring that all air that can exhale voluntarily from the lungs can be expelled.
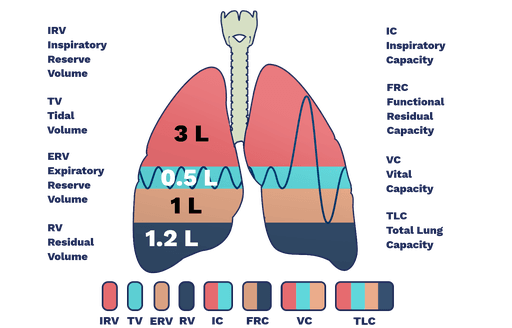
The vital capacity indicates the total volume of air, which can exhale after the deepest inhalation possible. It can be calculated as a total lung capacity the remaining size, which is the air that remains in the lungs after the strong exhalation. The remaining size cannot be expelled voluntarily, but it serves a vital role in preserving the vesicles (small air bags in the lungs) open and preventing lung breakdown.
Biomedical ingredients
To understand the vital ability more comprehensively, it is important to study the specific ingredients that contribute to this measurement. The vital capacity is the sum of many lung sizes that describe the air exchange during breathing. The main ingredients are:
- Tide size (television)
The tidal size indicates the amount of air that is inhaled or exhale during comfortable natural breathing. It is the smallest size involved in the respiratory cycle and is usually about 500 milliliters in an average adult in comfort. - Inspiring reserve size (IRV)
The size of the inspiring reserve is the maximum air that can be inhaled after natural inhalation. This represents the additional air that the lungs can take when performing a deep breath. - Exhale reserve size (ERV)
The size of the exhalation reserve is the maximum air size that can exhale after natural exhalation. Like IRV, ERV represents the additional size that the lungs can expel during forced breathing. - The remaining size (RV)
The remaining size is the air that remains in the lungs after the maximum exhalation. This folder is necessary because it prevents the vesicles from collapse and ensures that the gas is continuing even when the person does not breathe actively.
total Tide size (television)and Inspiring reserve size (IRV)And Exhale reserve size (ERV) It gives us vital total capacity:
Biomedia (VC) = TV + IRV + ERV
It is important to note that the remaining volume (RV) is not included in the vital capacity measurements because it cannot be exhaled out.
Lung capabilities
Lung capabilities are the terms used to describe the maximum air sizes that the lungs can carry. These capabilities include:
- Total lung capacity (TLC):
The total lung capacity indicates the maximum air that the lungs can carry after forced inspiration. In a healthy adult, TLC length is about 6000 ml. It can be calculated as follows:TLC = TV + Erv + Irv + RV - Biomedia (VC):
The vital capacity is the total volume of air that can be exhaled after the maximum inhalation or the maximum air that a person can breathe after an enforced validity. This is an important measure of a person’s respiratory health. A decrease in vital capacity may indicate Restriction lung diseaseWhere the lungs cannot fully expand. On the other hand, in Autoal lung diseases (For example, asthma or chronic obstructive pulmonary disease), the expansion of the lung is not the problem, but the air flow hinders in the airways. The vital ability is calculated as follows:Vc = TV + Erv + Irv - Inspiring ability (IC):
This is the total volume of air that can be inspired after the end of the normal validity, usually about 3600 ml. It is calculated as follows:IC = TV + Irv - The remaining functional power (FRC):
The remaining functional capacity indicates the size of the remaining air in the lungs after the natural exhalation, which is usually about 2,400 ml. It can be calculated as follows:FRC = Erv + RV
Domains and natural differences
The vital ability of healthy adults usually ranges between 3 and 6 liters, although this varies based on several factors. The main determinants of vital ability include:
- ageThe vital ability tends to decrease with a person’s progress due to lung flexibility loss.
- sexMales generally have a higher vital capacity than females, due to the differences in the size of the body and the size of the lung.
- to riseThe longest individuals tend to obtain greater lung capabilities and thus vital capabilities higher than shorter individuals.
The vital ability is reduced in both Blockage and restriction Lung diseases. In stubborn diseases such as asthma and Chronic obstructive pulmonary disease (chronic obstructive pneumonia)The airways become narrow, which makes the expulsion of the air more difficult. In restrictions, such as LibrantLung tissue becomes harsh, lung expansion restriction and reduces the total air that can be inhaled or exhale.
In addition, the vital capacity is associated with the level of disability in chronic respiratory diseases. With the deterioration of the lung function, a decrease in vital ability is often observed. Over time, VC monitoring can help evaluate the development of the disease and the effectiveness of treatments.
Types of vital capabilities
Biomedical ability can be evaluated in different ways, depending on the context of the test. Below are the most common types of vital capacity measers used in clinical practice:
- Vital forced exhalation abilities (FVC)
This test measures the total amount of air that a person can exhale strongly after taking a deep breath. FVC is usually measured in specific periods, such as one second (FVC1) or 3 seconds (FVC3). Forced end in a short period of time can highlight any blockage in the airways, making this test particularly useful in diagnosing lung lung diseases. - Slow vital ability (SVC)
The slow vital capacity test includes slow inhalation and air control. It measures the total volume of air, which can be inhaled and exhaled in a comfortable way. This type of measurement is especially useful in determining restricted lung diseases, as the lungs cannot fully expand due to solidity or scarring. - The ability of forced inspiration (FIC)
This test measures the total amount of air that a person can inhale fully after exhale. Such as forced validity, forced inspiration can help determine the conditions that reduce the ability to deeply inhale, such as restricted lung diseases.
Breathing
Measuring vital ability using a breathing scale
The vital capacity is commonly measured using a Breathing scaleIt is a device that records the size of the air inspired by the lungs. The breathing scale can accurately measure the different lung sizes, including the vital capacity, by tracking the amount of air that a person does in different conditions.
The vital ability measurement process with a breathing scale includes the following steps:
- to prepareA person who is tested is comfortable to sit comfortably or stand straight, ensuring his chest and stomach relaxation. If necessary, the nose may be cut to ensure that all exhale is air through the mouth.
- inhalationThe individual is required to take a deep inhalation, and to expand the lungs as much as possible.
- exhalationAfter inhalation, the person is required to exhale and complete it. During this process, the breathing scale measures the total size of the steady air.
- registrationThe respiratory scale records the total amount of air exhale (vital capacity), as well as additional measurements such as the time it takes to exhale and the airflow rate.
Additional measurements using a breathing scale
While breathing, many additional measurements are collected, which can provide more detailed visions of the lung function:
- Forced exhalation size in one second (FEV1):
FEV1 refers to the amount of atmosphere during the first second of the expiration of the forced validity. This is one of the most important measurements in breathing measurement because the FEV1 decrease can be an early mark on lung diseases such as Chronic obstructive pulmonary disease and asthma. A healthy person usually exhale most of the air in the first second, while individuals with airway blockage may have a slower exhalation rate. - Forced exhalation size in three seconds (FEV3):
Like Fev1, FEV3 measures the size of the air that was expelled during the first three seconds of forced exhalation. This measurement provides additional information about the blockage of air flow and can be used to assess the severity of lung disease. - The peak of exhalation flow (PEF):
The peak of the exhalation flow measures the highest flow rate that a person can achieve during the expiration of forced validity. It reflects exhale speed and is often used to monitor patients with asthma or other chronic respiratory cases. A decrease in PEF can indicate an exacerbation of the airway blockage. - The remaining size (RV):
The remaining size is the amount of air remaining in the lungs after a person completes forced exhalation. This folder cannot be measured directly by measuring breathing, but it is crucial in understanding the function of the total lung and can be measured using other techniques such as body planning.
The role of forced exhalation and forced vital ability in diagnosis
Mixture Forced exhalation size and Forced vital ability It plays a major role in the diagnosis and management of respiratory diseases:
- Diagnosis of chronic obstructive pulmonary disease:
the FEV1/FVC ratio (The ratio of forced exhalation in one second for forced biological ability) is a major scale in a diagnosis Chronic obstructive pulmonary disease (chronic obstructive pneumonia). FEV1 decrease with a decrease in the FEV1/FVC ratio to lung disease. Chronic pulmonary obstruction is characterized by restricting air flow, and the FEV1 decrease is the distinctive feature of this condition. - Lung disease monitoring:
the Fev1 The value can help doctors determine the stage of chronic obstructive pulmonary disease or other chronic lung diseases. It decreases in Fev1 Over time it can indicate that the disease gets worse. In contrast, improvements in FEV1 after medications or treatment may indicate that the lung condition settles or improves. - Evaluation of the effectiveness of treatment:
Forced vital capacity tests, along with FEV1 measurements, help assess the person’s response to bronchial confrontations or other drugs used to open airways in diseases such as asthma or chronic obstructive pulmonary disease. These measurements are especially important when controlling treatment plans or monitoring the effectiveness of inhalation and other therapeutic interventions.
The importance of observing biomed
Watching vital ability is an important tool for assessing lung health, especially for individuals with chronic respiratory diseases. Regular breathing measurement tests for healthcare providers allow tracking changes in lung function over time, help identify potential problems early and adjust treatment strategies. For example, in patients who suffer from asthmaMeasurement of vital capacity changes can help evaluate whether the exacerbation occurs and the effectiveness of asthma medications controls symptoms.
In addition to the clinical aspects, regular monitoring of the lung function in the population at risk-such as smokers, individuals who have a family history of the respiratory conditions, and those who suffer from professional exposure to materials that start the lung-can help capture lung diseases in their early stages. Early intervention can prevent more lung damage and improve long -term health results.
conclusion
Biomedia is a vital measure of lung health, which is crucial to diagnosing and monitoring respiratory diseases. It is affected by a range of factors, including age, gender, height and general health. By measuring vital ability through tests such as Vital forced exhalation abilities (FVC)and Slow vital ability (SVC)And The ability of forced inspiration (FIC)Healthcare providers can evaluate both lung diseases, blockage and restrictions. In addition, such as measurements Fev1and Fev3and PEFAnd The remaining size Provide a comprehensive picture of the lung function. Regular and continuous respiratory measurement tests are necessary to manage chronic respiratory cases and ensure patients with the optimum lung health.